## Robot-Assisted Dental Implant Surgery: A Comprehensive Overview This report from **Oral Health Group**, published on **October 10, 2025**, explores the burgeoning field of robot-assisted dental implant surgery, highlighting its evolution, capabilities, limitations, and future potential. The article, authored by Charlotte Fritz, a Master of Applied Science Candidate at the University of Toronto, details how artificial intelligence and robotics are transforming dental workflows, moving beyond administrative tasks to direct surgical intervention. ### Key Findings and Conclusions: * **Robotic assistance in dentistry is rapidly advancing**, with the potential to become mainstream for dental implant procedures. * **The Yomi Dental Robot**, developed by Neocis, is a significant development, being the first FDA-approved robotic guidance system for dental implant placement. * **By April 2025, over 70,000 dental implants had been placed using the Yomi robot**, indicating growing adoption. * Robotic systems offer **enhanced accuracy, consistency, and safety** in implant placement compared to traditional methods. * While robots excel at implant placement, they currently **struggle with auxiliary procedures** such as suturing, soft tissue management, and complex anatomical decision-making. * The **workflow for robot-assisted implant surgery involves detailed preoperative planning, patient and robot setup, robot-guided site preparation, implant placement, and postoperative verification.** * This advanced workflow can **enable immediate loading** of prosthetic restorations following implant insertion. * **Human-robot interaction is crucial**, with active and semi-active systems demonstrating higher accuracy and consistency than passive systems. * **Limitations include the risk of false confidence if initial planning is flawed, potential adverse events due to user error, and limited clinical data for long-term outcomes.** * The **high cost and physical size of robotic systems** may present barriers to widespread adoption. * The **future promises AI-powered surgical robots** with enhanced anatomical analysis, personalized treatment planning, intelligent control, and adaptive decision-making. ### Key Statistics and Metrics: * **July 2000:** Launch of the da Vinci Surgical System, proving the efficacy of robotic-assisted surgery. * **Sixteen years after da Vinci's launch (around 2016):** The Yomi Dental Robot became the first FDA-approved robotic guidance system for dental implant placement. * **April 2025:** More than **70,000 dental implants** had been placed using the Yomi robot. * **Single-tooth implant placements:** Approximately **20–25 minutes** using robotic assistance. * **Full-arch reconstructions:** Approximately **47–70 minutes** using semi-active robots. * **FDA Clinical Study:** Involved **44 implants** in **15 patients**, primarily conducted by general dentists in controlled environments. ### Types of Dental Implant Robots: Dental implant robots are classified based on their level of human-robot interaction: * **Active Robots:** Fully autonomous. The robot performs all steps, with the operator mainly monitoring and swapping drills. * *Example:* Yekebot * **Semi-Active Robots:** Partially autonomous. The robot handles site preparation and implant placement, but the operator guides its entry and exit. * *Example:* Remebot * **Passive Robots:** Controlled by the Surgeon. The robot provides mechanical guidance, but the surgeon performs all surgical steps. * *Example:* Yomi ### What is a Haptic Robot? A haptic robot is equipped with sensors and actuators that allow it to **provide and receive tactile (touch) and force feedback**. All three types of dental robots discussed are haptic robots. ### How Robots Differ from Static Guides or Dynamic Navigation: * **Static Guides:** Inexpensive, provide mechanical guidance. * **Dynamic Navigation:** Allows calibration of CT scans with 3D images on a screen for improved planning. * **Robots:** Offer responsive assistance during execution, including haptic feedback and compensation for patient movement, going beyond just planning. ### What Robots Can Do in 2025: * Excel at **implant placement with a flapless approach**. * Struggle with **suturing, soft tissue management, complex anatomical decision-making, and auxiliary surgeries** like GBR and sinus lifts. ### Promises of Robotic Assistance: * **Accuracy:** More accurate than freehand, guides, or dynamic navigation, with greater stability in drill orientation and compensation for patient motion. * **Consistency:** Standardizes surgical movements, reducing variability and cognitive demands on the surgeon. * **Safety:** Controls drill depth, angle, and trajectory, minimizes soft tissue trauma, and includes integrated sensors and safety stops. * **Efficiency:** Easier cost forecasting, avoidance of postponed procedures, facilitation of complex cases, and elimination of the need for plastic drill guides. ### Workflow of Robot-Assisted Implant Surgery: 1. **Preoperative Planning:** Acquire CBCT and intraoral scans, plan implant position, angulation, and depth. 2. **Patient and Robot Setup:** Position patient, attach tracking markers, register anatomy with the digital plan, and calibrate the robotic arm. 3. **Robot-Guided Site Preparation:** Robot locks in the desired implant placement axis, and drills the osteotomy along the pre-planned trajectory, compensating for patient movement. 4. **Implant Placement:** Robot places the implant to the programmed depth and angle, with surgeon supervision and the ability to override. 5. **Postoperative Verification:** Remove equipment, acquire radiographic imaging to confirm position, and compare planned vs. achieved outcomes. ### Clinical Benefits & Findings: * **Greater Flexibility:** Enhanced access, visibility, irrigation, and real-time plan modifications. * **Human-Robot Interaction Matters:** Active and semi-active systems show high accuracy across operators; passive systems have greater variability. * **Limits in Auxiliary Procedures:** Robots are not capable of grafting, sinus lifts, flap reflection, or suturing. * **Higher Implant Placement Accuracy:** Significantly improves accuracy compared to freehand techniques, especially for fully and partially edentulous cases. * **Comparable Surgical Time:** Robotic procedures generally require similar operative time to freehand methods. ### Limitations & Considerations: * **Accuracy vs. Precision:** Precision is validated, but accuracy (achieving the "ideal" restorative-driven position) is not guaranteed, especially in complex cases. * **Risk of False Confidence:** The robot precisely replicates the surgeon's chosen trajectory, which can be problematic if the initial assessment is flawed. * **Potential Adverse Events:** User error can lead to adverse events, highlighting the importance of surgeon skill and vigilance. * **Differences in Bone Density:** Can lead to robotic arm movement and deviations. * **Limited Clinical Data:** More high-quality clinical trials are needed to validate safety and long-term efficacy. * **Contraindications:** Not suitable for cases with questionable bone volume or proximity to vital structures. * **Cost and Practicality:** High cost, large size, and setup time can limit adoption. * **Patient Acceptance:** Motivation for robotic therapy decreases as procedure invasiveness increases. ### The Future: Next-generation AI-powered surgical robots are expected to: * **Enhance anatomical analysis** and identify optimal implant sites. * Enable **personalized treatment planning**. * Improve **outcome verification** and track accuracy. * Provide **intelligent robotic control** with adaptive decision-making. * Integrate with **smart learning systems** for continuous performance improvement, potentially leading to semi-autonomous or fully autonomous implant placement. Despite these advancements, **clinicians must continue to provide oversight**, with ethical considerations, patient safety, and surgeon judgment remaining paramount.
From AI in the office to robot-assisted dental implant surgery - Oral Health Group
Read original at Oral Health Group →iStock ChatGPT has transformed your admin workflows and treatment notes. Now, meet the robots entering your operatory.1 1. The rise of surgical robotics When the da Vinci Surgical System launched in July 2000, it proved to general surgeons that robotic-assisted surgery, offering high-definition 3D views and built-in tremor-filtration technology, could be effectively applied to a wide range of procedures, including for cardiovascular, colorectal and general surgery.
2 Because the robot’s instruments are able to fit through small incisions, robot surgery is less invasive than open surgery, and in many cases results in fewer post-op side effects and shorter recovery times for patients.3 Sixteen years later, the Yomi Dental Robot—developed by start-up Neocis—became the first robotic guidance system approved by the FDA for dental implant placement.
4 By April 2025, Neocis reported that more than 70 000 dental implants had been placed using the robot.5 While robotic assistance in dentistry is still far from ubiquitous, it seems that the once dystopian notion of it being mainstream for robots to perform dental implant surgical procedures is no longer a matter of if, but when.
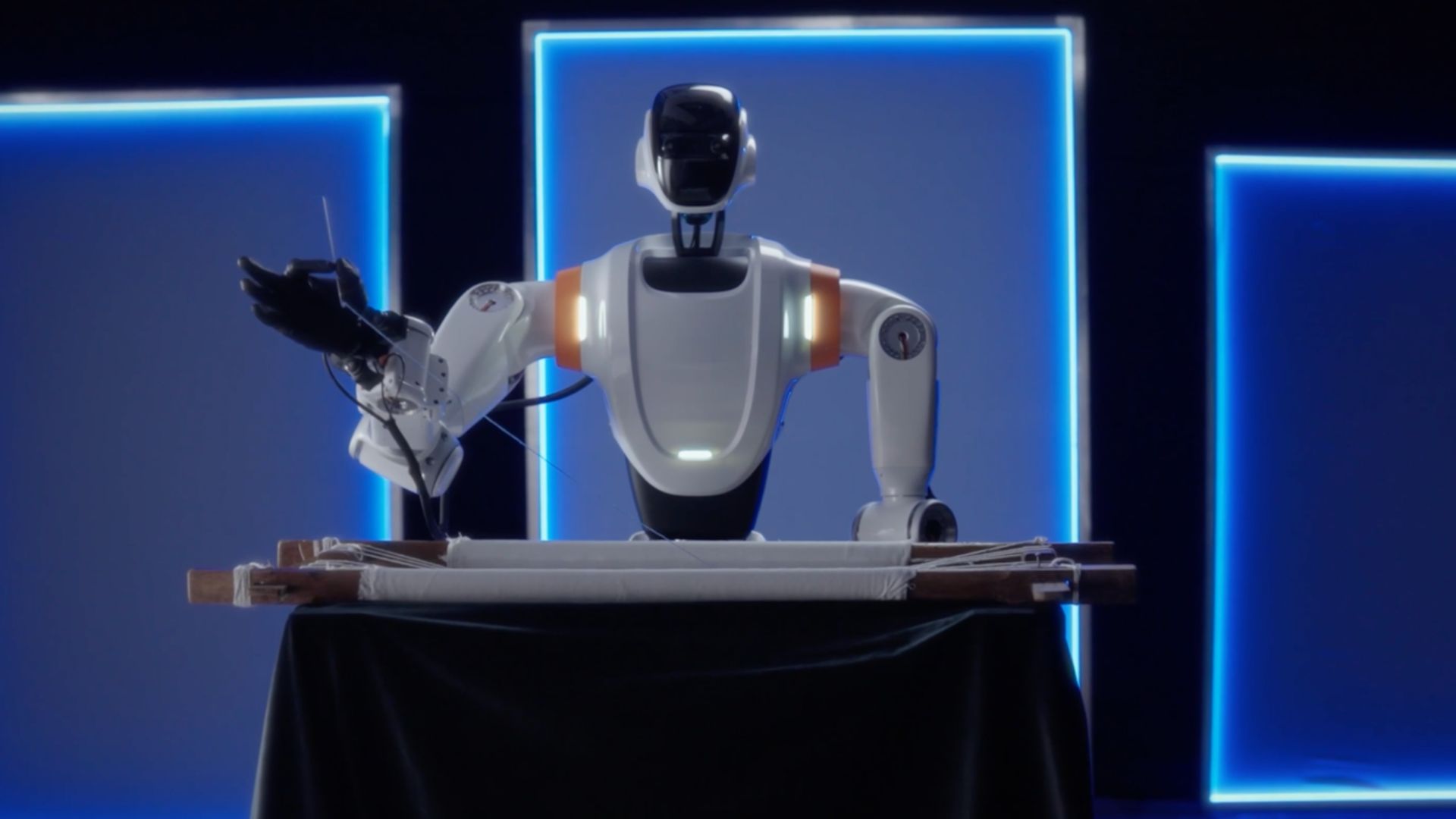
2. What exactly is a dental implant robot? Not unlike how a dentist uses their hands, eyes, and brain to perform surgery, today’s dental implant robots use a robotic operation platform to manipulate instruments, a vision system for spatial awareness, and a central control system to interface the two, continually adjusting the instrument based on the spatial updates received.
6 Dental implant robots are classified based on the level of human-robot interaction involved with operation7: Active Robots6,7 – Fully autonomous The robot enters/exits the mouth, prepares the implant site, and places the implant. The operator mainly monitors and swaps drills. Example: Yekebot7 Semi-Active Robots6,7 – Partially autonomous The robot handles site preparation and implant placement, but the operator guides its entry and exit into the mouth.
Example: Remebot7 Passive Robots6,7 – Controlled by Surgeon The robot provides mechanical guidance, but the surgeon handles entry/exit, site preparation, and implant placement. Example: Yomi7,8 What is a haptic robot? A haptic robot is equipped with sensors and actuators that enable it to provide and receive tactile (touch) and force feedback.
8,9 All three types of dental robots presented above are haptic robots. How is a robot different from a static guide or dynamic navigation? Both static guides and the increasing popularity of dynamic navigation speak to a larger shift in the industry towards solutions that offer greater precision and control.
Static guides are inexpensive; dynamic navigation allows the implant surgeon to calibrate a patient’s CT scan in alignment with a 3D image on a navigation screen.10 Both technologies improve the planning of dental implant surgery, but a robot can also provide responsive assistance during execution through providing haptic feedback, including in response to patient movement.
7 What can robots do in 2025? Current robots excel at implant placement with a flapless approach, but struggle with suturing, soft tissue management, complex anatomical decision-making and auxiliary surgeries such as GBR and sinus lifts.6 3. What robotic assistance promises Accuracy More accurate than freehand, guides, or dynamic navigation.
5 Provide greater stability in maintaining drill orientation via the robotic arm (prevent slipping off a ridge of bone or into an extraction socket or soft bone).11,12 Able to compensate for intraoperative patient motion via visual feedback and live imaging, improving surgical awareness and precision.
7,13 Consistency Standardizes surgical movements via system calibration and registration, reducing variability between procedures and among different clinicians.14 Reduces physical and cognitive demands on the surgeon, helping to maintain procedural quality.6,14 Safety Controls drill depth, angle, and trajectory to avoid critical anatomical structures.
Minimizes back and neck pain for the clinician.14,15 Reduces soft tissue trauma and postop complications by increasing implant placement precision; do not have to open the gums to surgically place the robot.8 Halts drilling if deviations from the plan are detected; system is integrated with sensors and safety stops.
11 Efficiency (i.e. operation and preparation time) Easier to forecast costs and avoid postponed procedures.11,16 Facilitates complex cases (full-arch cases) by lowering fatigue and enabling parallelism.11,17 Eliminates need for plastic drill guides, which can block irrigation from or visibility of the surgical site.
18 4. Workflow of robot-assisted implant surgery The following is a general overview of the workflow associated with today’s dental implant robots: Step 1: Preoperative planning Acquire CBCT (Cone Beam Computed Tomography) and intraoral scans on the day of surgery to generate a 3D map of the patient’s anatomy.
5,20 Plan implant position, angulation, and depth within the robotic software.5,19,20 Consider prosthetic design, bone density, and proximity to anatomical structures (sinus, nerve canals).5,19,20 Step 2: Patient and robot setup Position the patient and attach tracking markers (intra-oral splint, screws) for registration.
5,19,20 Register the patient’s anatomy with the digital plan to align the robot.19 Calibrate the robotic arm and confirm all surgical tools are functional by correctly locating the patient’s structures by touching a preselected landmark with the robot’s end effector (instrument).20 Step 3: Robot-guided site preparation Operator advances end effector close to the surgical site and robot will lock in the desired implant placement axis, and will only allow vertical movement by the surgeon.
20 Robot drills the osteotomy along the pre-planned trajectory.19,20 Real-time tracking compensates for patient movements during surgery.5 Step 4: Implant placement Robot places the implant to the pre-programmed depth and angle.5,19 The surgeon supervises and can override the robot if needed; throughout the procedure, the surgeon has control of the progress of the drill in the axis of the osteotomy.
20 Shared control ensures precision while maintaining clinical judgment.5,19,20 Step 5: Postoperative verification Remove robotic equipment and trackers after placement.5,20 Acquire postoperative radiographic imaging to confirm implant position.5,20 Compare planned versus achieved outcomes; document deviations for accuracy assessment.
5,19,20 Can workflow precision enable immediate loading? One study demonstrated that the implementation of this workflow achieves a level of precision in implant placement that permits the prosthetic restoration to be fabricated in advance of surgery, thereby facilitating immediate loading following implant insertion.
20 5. Clinical benefits & findings Greater flexibility Robotic workflows enhance access, visibility, and irrigation, especially in anatomically challenging or posterior regions.6,9 They also permit intraoperative plan modifications, giving clinicians the ability to adjust trajectory or angulation in real-time without discarding physical guides.
6,9 Human–robot interaction matters Implant precision is not only a function of the robot, but also of the mode of collaboration between surgeon and machine. Active and semi-active systems consistently maintain high accuracy across operators and procedures.6 By contrast, passive robotic systems show greater variability, with accuracy more dependent on surgeon skill and consistency.
6 Limits in auxiliary procedures Robotic systems demonstrate strong precision in osteotomy and implant insertion.7 They are not capable of performing grafting, sinus lifts, flap reflection, or suturing.7 These auxiliary procedures require delicate soft tissue handling and intraoperative adaptability that remain beyond current robotic capability.
7 Higher implant placement accuracy Robot-assisted implant placement significantly improves implant accuracy compared to freehand techniques, including cases requiring bone grafting for narrow alveolar crests.12,14 Fully and partially edentulous cases are identified as prime candidates for robot assisted surgery.
20 Comparable surgical time Robot-assisted procedures generally require similar operative time compared to freehand. Reported times: Single-tooth placements: ~20–25 minutes. Full-arch reconstructions: ~47–70 minutes (using semi-active robots). Thus, the precision benefits of robotics do not appear to significantly extend chairside duration.
7 Taken together, these findings suggest that robotic surgery can successfully support immediately loaded implants, and allow precise, minimally invasive, and patient-specific procedures.19 However, more clinical trials are needed to confirm efficacy and long-term outcomes.7 6. Limitations & considerations Accuracy versus Precision Precision is validated, but accuracy is not guaranteed.
11 This means the system may not achieve the “ideal” restorative-driven implant position, especially in complex cases.11 Risk of false confidence The robotic arm maintains the surgeon-defined trajectory with high repeatability, which may create a false sense of accuracy.11 If the starting trajectory is poorly chosen (due to limited anatomical assessment), the robot will precisely replicate an imprecise plan.
11 Potential adverse events Adverse events have been reported (implant displaced into the sinus during hand-torquing).11 Root cause was found to be user error, but highlights the importance of surgeon skill and vigilance even when using robotic assistance.11 Differences in buccal and palatal bone density have led to robotic arm movement and greater apical deviations in fresh extraction sites.
7 Limited clinical data FDA clinical study: only 44 implants in 15 patients.11 Conducted mainly by general dentists in controlled environments.11 Long-term outcomes (osseointegration, prosthetic complications, biomechanical implications of angular deviation) are still not fully studied.11 Many studies are in vitro or on simple cases; more high-quality clinical trials are needed to validate safety and long-term efficacy.
6 Contraindications Not suitable where bone volume or proximity to vital structures is questionable.11 Cost and practicality High cost, large physical size, and setup time may limit adoption; efficiency gains depend on operator experience.20 Patient acceptance Motivation for robotic therapy decreases for all patients as procedure invasiveness increases.
21 7. The future Next-generation AI-powered surgical robots promise to transform dental implantology by combining advanced computational intelligence with robotic precision.22 Potential capabilities include: Enhanced anatomical analysis: Automatically analyze CBCT scans to identify optimal implant sites, assess bone density, and highlight critical structures.
23 Personalized treatment planning: Design implant plans tailored to each patient’s anatomy and prosthetic requirements.23 Outcome verification: Compare preoperative and postoperative scans to track accuracy, deviations, and long-term results.24 Intelligent robotic control: Dynamically adjust movements during surgery to maintain precision, compensate for unforeseen conditions, and reduce human error.
7 Adaptive decision-making: Respond in real time to intraoperative changes, enhancing safety and procedural efficiency.7 Integration with smart learning systems: Leverage accumulated procedural data to continuously improve performance, potentially enabling semi-autonomous or fully autonomous implant placement in the future.
7 While these advances hold promise for unprecedented precision and efficiency, clinicians must continue to provide oversight. Ethical considerations, patient safety, and the surgeon’s judgment remain paramount as autonomous capabilities evolve. Oral Health welcomes this original article. AI Disclosure: Initial brainstorming, assisting in the understanding of high-concept ideas, and portions of text refinement were supported by OpenAI’s GPT-5 language model.
The AI was used exclusively for editorial purposes such as language clarity. All clinical content, use of external research articles, interpretations, and conclusions were independently developed and verified by the author. References H. M. Alhaidry, B. Fatani, J. O. Alrayes, A. M. Almana, and N. K.
Alfhaed, “ChatGPT in Dentistry: A Comprehensive Review,” Cureus, vol. 15, no. 4, Apr. 2023, doi: https://doi.org/10.7759/cureus.38317. Intuitive, “Robotic-Assisted Surgery with Da Vinci Systems,” Intuitive.com, 2023. https://www.intuitive.com/en-us/patients/da-vinci-robotic-surgery Cleveland Clinic, “da Vinci Surgery: Treatment & Recovery,” Cleveland Clinic, May 24, 2021.
https://my.clevelandclinic.org/health/treatments/16908-da-vinci-surgery “The Latest in Dental Robotics,” constituent. https://www.agd.org/constituent/news/2023/04/17/the-latest-in-dental-robotics Yomi by Neocis, “What is Yomi? A robotic platform that’s revolutionizing dental implant surgery,” YouTube, Mar.
07, 2025. https://www.youtube.com/watch?v=BIfrwNoztzg (accessed Sep. 01, 2025).11466, May 20, 2022. Z. Xu et al., “Accuracy and efficiency of robotic dental implant surgery with different human-robot interactions: An in vitro study,” Journal of Dentistry, vol. 137, pp. 104642–104642, Oct. 2023, doi: https://doi.
org/10.1016/j.jdent.2023.104642. R. Bahrami, M. Pourhajibagher, Nariman Nikparto, and Abbas Bahador, “Robot-assisted dental implant surgery procedure: A literature review,” Journal of dental sciences, Mar. 2024, doi: https://doi.org/10.1016/j.jds.2024.03.011. “Robot-Guided Dental Implant Surgery – See The Yomi Robot,” Yomi By Neocis.
https://www.neocis.com/products-and-services/yomi-robot/ Almira Isufi, T.-Y. Hsu, and Sami Chogle, “Robot Assisted and Haptic Guided Endodontic Surgery: A case report,” Journal of Endodontics, Jan. 2024, doi: https://doi.org/10.1016/j.joen.2024.01.012. N. Panchal, L. Mahmood, A. Retana, and R. Emery, “Dynamic Navigation for Dental Implant Surgery,” Oral and Maxillofacial Surgery Clinics of North America, vol.
31, no. 4, pp. 539–547, Nov. 2019, doi: https://doi.org/10.1016/j.coms.2019.08.001. Neocis Inc., “K211466: Premarket Notification—Yomi Robotic System with YomiPlan Go,” U.S. Food & Drug Administration, Silver Spring, MD, FDA K-number K211466, May 20, 2022. S. Jain et al., “Accuracy Comparison between Robot-Assisted Dental Implant Placement and Static/Dynamic Computer-Assisted Implant Surgery: A Systematic Review and Meta-Analysis of In Vitro Studies,” Medicina (Kaunas, Lithuania), vol.
60, no. 1, p. 11, Dec. 2023, doi: https://doi.org/10.3390/medicina60010011. “Robotic Systems and Dental Implants | Oakville, ON, Best Implant Dentist Near You,” Dental Implants in Oakville, Oct. 31, 2017. https://dentalimplantsinoakville.com/dental-implants-news/robotic-systems-and-dental-implants/ (accessed Aug.
25, 2025). J. Chen et al., “Accuracy, Safety, and Efficiency in Robotic-Assisted vs. Freehand Dental Implant Surgery: A 6-Month Follow-Up Randomized Controlled Trial,” Clinical oral implants research, vol. 36, no. 5, pp. 662–670, May 2025, doi: https://doi.org/10.1111/clr.14413. S. Yang, J. Chen, A.
Li, P. Li, and S. Xu, “Autonomous Robotic Surgery for Immediately Loaded Implant-Supported Maxillary Full-Arch Prosthesis: A Case Report,” Journal of Clinical Medicine, vol. 11, no. 21, p. 6594, Nov. 2022, doi: https://doi.org/10.3390/jcm11216594. “Robot-Guided Dental Implant Surgery – See The Yomi Robot,” Yomi By Neocis.
https://www.neocis.com/products-and-services/yomi-robot/ B. Sobczak and P. Majewski, “An Integrated Fully Digital Prosthetic Workflow for the Immediate Full-Arch Restoration of Edentulous Patients—A Case Report,” International Journal of Environmental Research and Public Health, vol. 19, no. 7, p. 4126, Mar.
2022, doi: https://doi.org/10.3390/ijerph19074126. “Robotic Systems and Dental Implants | Oakville, ON, Best Implant Dentist Near You,” Dental Implants in Oakville, Oct. 31, 2017. https://dentalimplantsinoakville.com/dental-implants-news/robotic-systems-and-dental-implants/ (accessed Aug. 25, 2025).
S. Yang, J. Chen, A. Li, P. Li, and S. Xu, “Autonomous Robotic Surgery for Immediately Loaded Implant-Supported Maxillary Full-Arch Prosthesis: A Case Report,” Journal of Clinical Medicine, vol. 11, no. 21, p. 6594, Nov. 2022, doi: https://doi.org/10.3390/jcm11216594. Serge Dibart, Jeremy Kernitsky Barnatan, Massimo Di Battista, and L.
Montesani, “Robot Assisted Implant Surgery: Hype or Hope?,” Journal of Stomatology, Oral and Maxillofacial Surgery, pp. 101612–101612, Aug. 2023, doi: https://doi.org/10.1016/j.jormas.2023.101612. P. Ahmad et al., “Dental Robotics: A Disruptive Technology,” Sensors, vol. 21, no. 10, p. 3308, May 2021, doi: https://doi.
org/10.3390/s21103308. E. Veseli, “The future of dentistry through robotics: Artificial intelligence,” British Dental Journal, vol. 238, no. 2, pp. 76–77, 2025, doi: 10.1038/s41415-025-8345-8. V. Reed, “AI In Dentistry: The Rise Of Robot Dentists,” AI Proficiency Hub #AICompetence.org, Aug. 07, 2024.
https://aicompetence.org/ai-in-dentistry-the-rise-of-robot-dentists/ L. M. Nassani, K. Javed, R. S. Amer, M. H. J. Pun, A. Z. Abdelkarim, and G. V. O. Fernandes, “Technology Readiness Level of Robotic Technology and Artificial Intelligence in Dentistry: A Comprehensive Review,” Surgeries, vol. 5, no.
2, pp. 273–287, 2024, doi: 10.3390/surgeries5020025. About the author Charlotte Fritz is a current Master of Applied Science (MASc) Candidate at the University of Toronto. She previously completed her Bachelor of Applied Science (BASc) in Computer Engineering. Her passion lies in leveraging engineering design to enhance cybersecurity in critical sectors, including healthcare, financial services, and industrial systems.